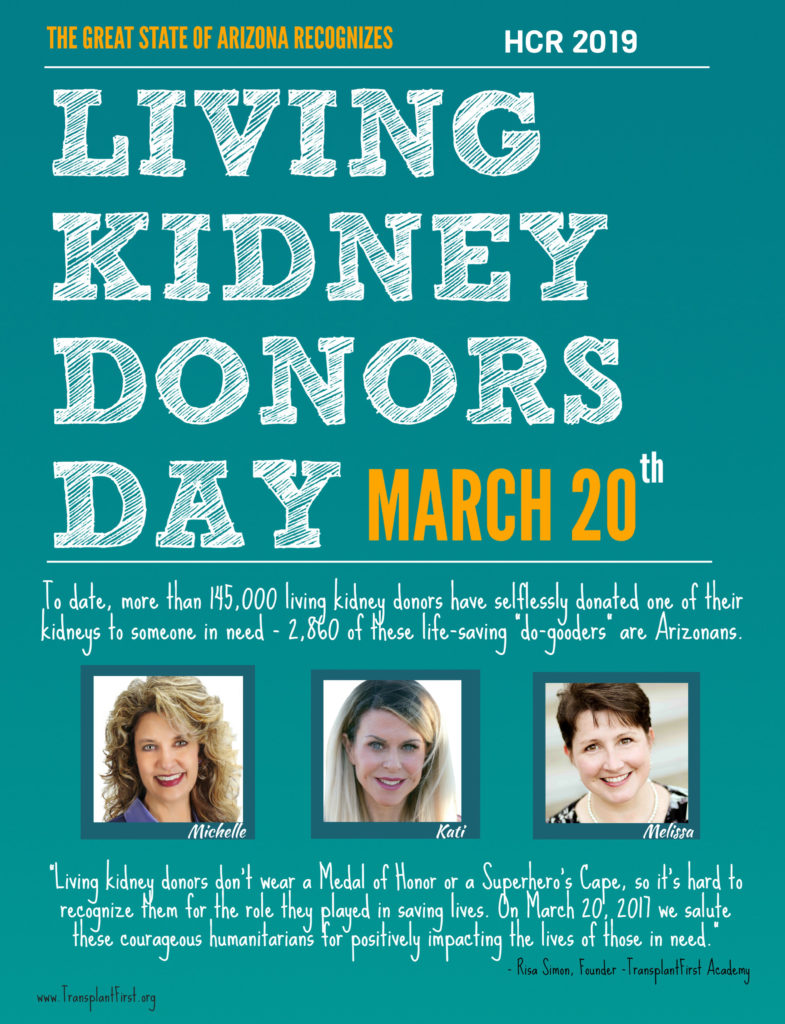
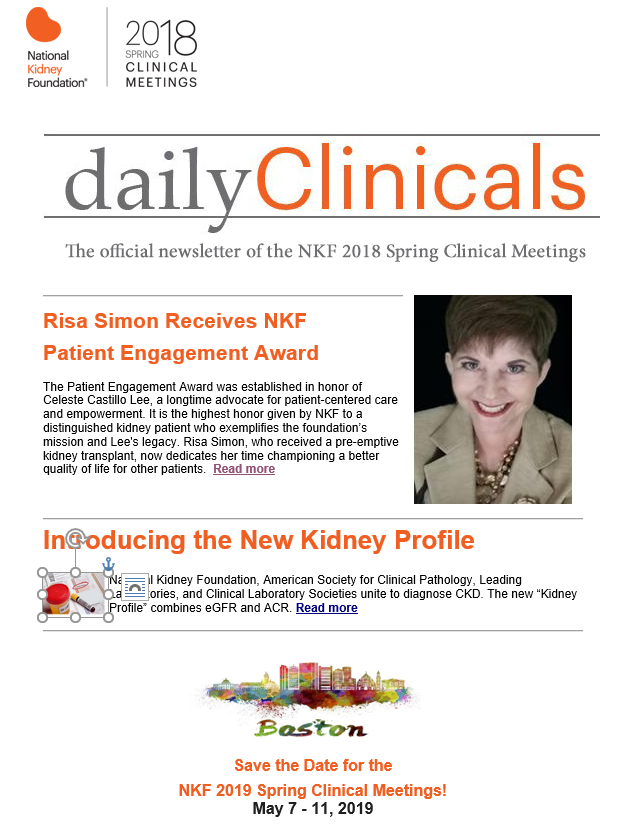
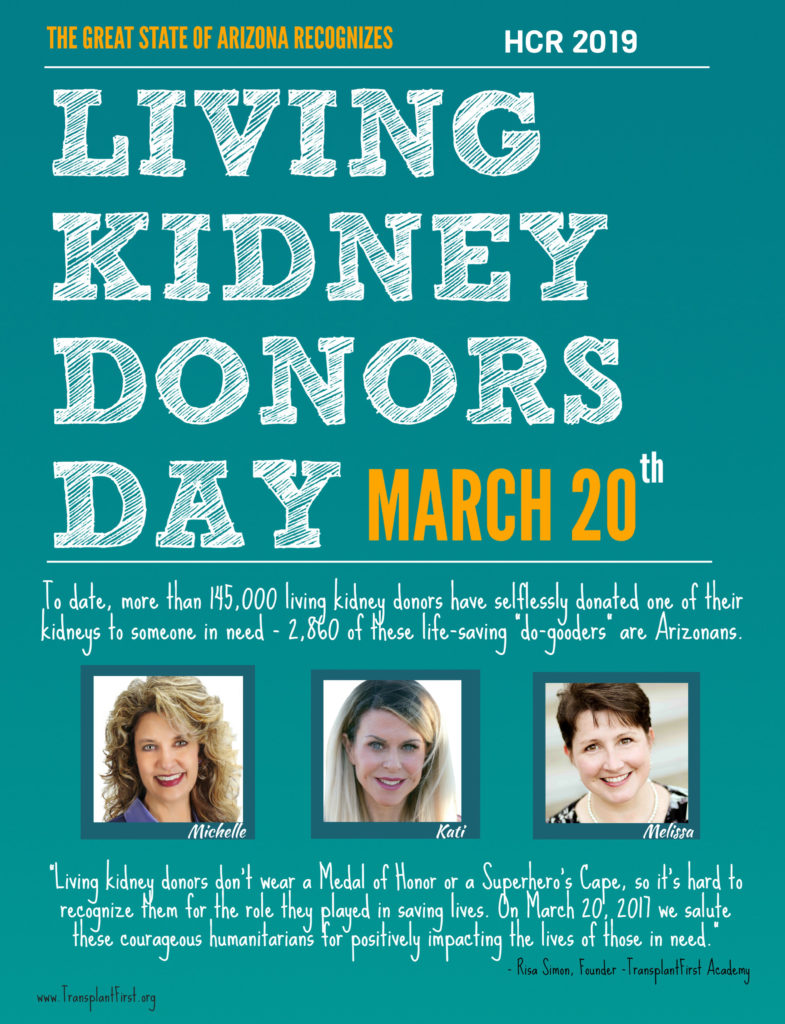
The state of Arizona’s proclamation HCR 2019 recognizes Living Kidney Donors Day, as the first state in the nation to recognize Living Kidney Donors for their selfless humanitarianism. Of course, we owe a great deal of gratitude to Arizona Representative Heather Carter, R-Cave Creek, who teamed up with Kati Walker, media spokesperson for the TransplantFirst Academy (TFA) and proclamation’s brainchild and TFA’s founder, Risa Simon, for creating this well-deserved day of tribute.
On March 20th, we ask you to reach out and honor all living kidney donors (LKDs) who donated a kidney to save and extend the life of someone in need. LKD’s not only save lives, they give hope to who are waiting for a kidney from a deceased organ donor, which often takes 3-5 years. They also inspire ordinary people to seek extraordinary opportunities, by contributing to one of the most amazing, once-in-a-lifetime achievements available on this planet!
Living Kidney Donors Day helps us remember these humble heroes, which is important since LKD’s don’t wear a Medal of Honor or a superhero’s cape. They don’t hold a sign or carry a badge. In fact, they don’t even claim to be heroes. Yet, we know otherwise by observing the remarkable outcomes as a result of the lives they saved.
Living Kidney Donors Deserve More Recognition
We believe living kidney donors deserve more recognition. The intention of this campaign is to do just that, by publicly honoring these remarkable humanitarians, as extraordinary human beings who selflessly donated one of their kidneys to end the life-threatening wait for someone in need.
Living kidney donors are individuals who chose to donate a kidney (sometime during their lifetime) after obtaining approval from a transplant center’s medical evaluation committee. Most living donors choose to donate because they either knew someone in need or simply wanted to help a stranger.
Witness the Miracle
Because living kidney donors choose to donate one of their kidneys while they are living,* they get to witness the miracle of their gift (and experience immense pride of accomplishment) for years to come. *Living kidney donors also retain their right to donate their remaining organs later in life.
Just Imagine
Ever imagined what it would be like to save someone’s life or improve the quality of someone’s life by extending their remaining years- while you are still alive? Living kidney donors have transformed this dream into reality.
In this campaign, we’re inviting real-life living kidney donors to show their proud faces, take a bow and elevate their story to help us increase awareness and inspire others to lean in this direction. Have they inspired you?
Hidden Organ Donor Facts:
The Need: Over 109,000 end-stage kidney disease patients are in desperate need of a replacement kidney.
The Wait: It can take 3 to 9 years to receive the gift of a kidney from a deceased organ donor on the national transplant list. Living Kidney Donation can end the wait.
The Benefit: Kidney transplants offer a far better alternative to dialysis. The benefits include, a better quality-of-life, fewer medical complications and longer survival rates.
Match-Making: Living kidney donors don’t have to be blood-related to the recipient. They only need to be blood-type compatible. But even then, there are Paired Exchange Programs that can offer alternatives.
Know Your (ABO) Blood-Type
Your blood-type is necessary to determine if you’ll be blood-type compatible to the person in need. You can either ask your doctor for a blood-type (ABO) test or seek a “direct-consumer” lab alternative. Direct-consumer labs allow patients to order lab tests with or without a doctor’s order. Thanks to House Bill 2645 (sponsored by Arizona Representative Heather Carter, R-Cave Creek and approved by Gov Doug Ducey) this bill now allows consumers in Arizona the ability to request basic lab tests and access results through a secure online portal.
The Opportunity: Healthy individuals can donate a kidney while they are still living and continue to live a full life. In other words, kidney donors don’t have to wait until after they’ve passed to donate. They do, however, need to pass the transplant center’s donor qualification process in order to proceed.
Learn As Much As You Can
There’s a lot to discover when it comes to living kidney donation. That’s why we created the Top Twelve “Need to Know” Answers to the most frequently asked questions on living kidney donation. We encourage you to take the time to explore this handout. Learn more here: See Top Twelve Questions on LKD.










 Many kidney disease patients are floating in a sea of uncertainty due to inadequate patient education and various knowledge barriers. Consequently, the patient’s understanding of various treatment options and outcomes—and how the timing of engagement can impact each outcome, is often lost in the shuffle of care. With the clock ticking behind the scenes, the patient’s inability to trigger optimal timing for best outcomes remains far beyond the scope of their awareness and comprehension.
Many kidney disease patients are floating in a sea of uncertainty due to inadequate patient education and various knowledge barriers. Consequently, the patient’s understanding of various treatment options and outcomes—and how the timing of engagement can impact each outcome, is often lost in the shuffle of care. With the clock ticking behind the scenes, the patient’s inability to trigger optimal timing for best outcomes remains far beyond the scope of their awareness and comprehension.